- Understanding-Oral-Fungal-Infection
- Key-Signs-and-Symptoms
- Causes-and-Risk-Factors
- Real-Life-Cases-and-Insights
- Prevention-and-Treatment-Options
- Professional-Care-and-Support
1. Understanding Oral Fungal Infection
Oral fungal infections, often known as oral thrush or candidiasis, occur when there is an overgrowth of fungus in the mouth, most commonly Candida albicans. This condition can affect people of all ages and backgrounds but tends to be more prevalent among those with weakened immune systems, infants, and older adults. Understanding the nature of oral fungal infections is crucial to identifying signs of oral fungal infection symptoms early, which can prevent complications and promote faster recovery.
Unlike bacterial infections, fungal infections may not always be painful at first, making it easy to overlook early symptoms. However, timely recognition can help manage the infection before it spreads or worsens.
1.1 The Role of Candida in the Mouth
Candida species are natural inhabitants of the oral cavity, usually kept in balance by the immune system and beneficial bacteria. When this balance is disrupted, Candida can multiply uncontrollably, leading to the development of candidiasis. This imbalance may be triggered by various factors such as antibiotic use, diabetes, dry mouth, or immune suppression.
1.2 Differentiating Oral Fungal Infection from Other Oral Issues
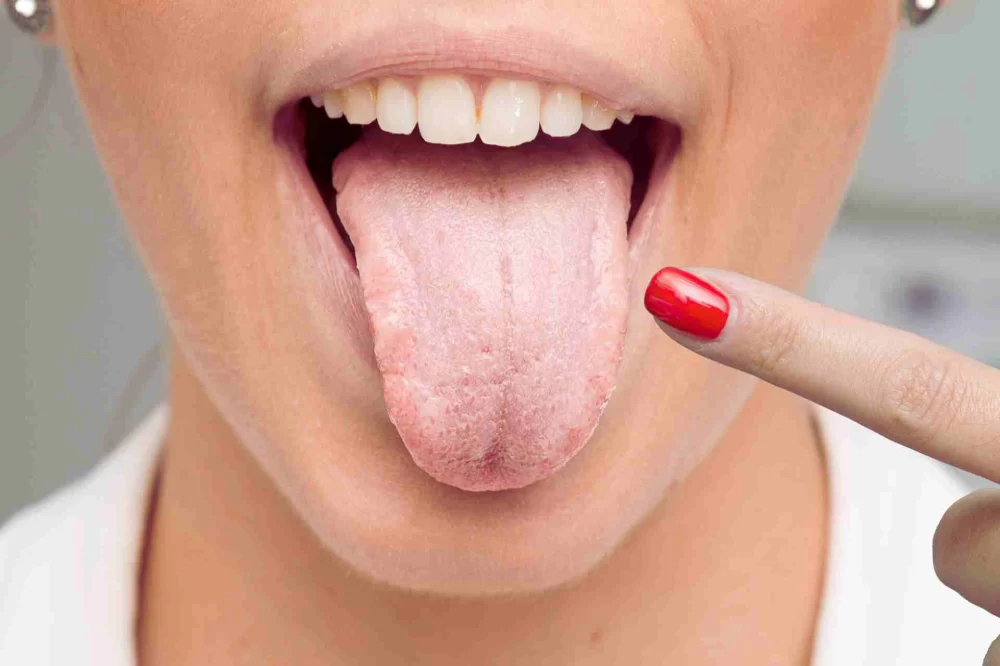
Many oral conditions share symptoms like redness, soreness, or white patches. Knowing the distinct characteristics of oral fungal infection helps avoid misdiagnosis. For example, unlike simple irritation or canker sores, oral thrush typically presents with creamy white lesions that can be wiped off to reveal a red, sometimes bleeding surface beneath.
2. Key Signs and Symptoms of Oral Fungal Infection
Recognizing the early and advanced signs of oral fungal infection symptoms is essential for timely intervention. The symptoms can vary based on the infection's severity and the individual’s overall health.
2.1 Common Symptoms
The hallmark signs include white, creamy patches on the tongue, inner cheeks, roof of the mouth, gums, and tonsils. These patches might resemble cottage cheese but can be easily scraped off, leaving a red, inflamed area underneath. Other symptoms include:
- A burning sensation or soreness in the mouth or throat
- Difficulty swallowing or a feeling of food being stuck
- Cracking and redness at the corners of the mouth, also known as angular cheilitis
- Loss of taste or an unpleasant taste in the mouth
- Dry mouth or increased salivation
2.2 Less Common Symptoms and Complications
In more severe cases, the infection can spread beyond the oral cavity, affecting the esophagus or other parts of the digestive tract, causing more significant discomfort and requiring urgent medical attention.
3. Causes and Risk Factors Behind Oral Fungal Infections
Identifying what triggers oral fungal infections can help prevent their occurrence and guide effective treatment. Several factors contribute to the overgrowth of Candida in the mouth.
3.1 Common Causes
The most frequent cause is the disruption of normal oral flora due to:
- Use of antibiotics or corticosteroids
- Poor oral hygiene
- Wearing dentures that don’t fit properly or are not cleaned regularly
- Dry mouth conditions caused by medications or diseases
- Smoking, which alters the oral environment
3.2 Health Conditions Increasing Susceptibility
People with weakened immune systems, such as those with HIV/AIDS, cancer patients undergoing chemotherapy, or diabetics with uncontrolled blood sugar levels, are more vulnerable. Additionally, infants and the elderly often face higher risks due to less robust immune defenses.
4. Real-Life Cases and Insights
To bring these signs and symptoms into perspective, consider the story of Jane, a 55-year-old diabetic patient who initially dismissed her mild discomfort and white patches as mere irritation. Over weeks, the patches grew, and she experienced increased soreness and difficulty eating. After visiting a dental professional, Jane was diagnosed with oral candidiasis. Early treatment helped her recover quickly, but her case highlights the importance of not ignoring signs of oral fungal infection symptoms.
Such real-life cases underline the necessity for vigilance, especially among at-risk groups, and reinforce why professional evaluation is crucial when unusual oral symptoms appear.
5. Prevention and Treatment Options
Prevention focuses on maintaining a healthy oral environment and immune system. This includes good oral hygiene, proper denture care, balanced nutrition, and managing underlying health issues like diabetes.
5.1 Treatment Approaches
Treatment typically involves antifungal medications, either topical (such as lozenges or mouth rinses) or systemic (oral tablets), depending on severity. It’s important to follow medical advice closely to prevent recurrence. Home remedies, such as rinsing with saltwater or maintaining hydration, can support healing but should not replace professional treatment.
5.2 The Role of Professional Dental Care
Regular dental check-ups can identify early signs of oral fungal infection symptoms before they develop into more serious conditions. Dental professionals can also recommend suitable oral care products and personalized advice tailored to individual risk factors.
6. Professional Care and Support Available
If you suspect you have an oral fungal infection, seeking timely professional support is key. Dentistry Toothtruth offers comprehensive evaluations and tailored treatment plans designed to tackle oral thrush and other fungal infections effectively. Their experts also guide patients on preventive strategies, ensuring sustained oral health and comfort.
With proper care and attention, most oral fungal infections can be managed successfully, allowing patients to enjoy pain-free oral function and improved quality of life.







 TruYou Dental - Franklin Lakes4.0 (778 review)
TruYou Dental - Franklin Lakes4.0 (778 review) Northpark Dental4.0 (99 review)
Northpark Dental4.0 (99 review) Family Dentistry of Westford4.0 (19 review)
Family Dentistry of Westford4.0 (19 review) Perfect Teeth Dental & Orthodontics - Olive4.0 (384 review)
Perfect Teeth Dental & Orthodontics - Olive4.0 (384 review) Nordstrom Orthodontics - Johnston4.0 (69 review)
Nordstrom Orthodontics - Johnston4.0 (69 review) Orchard Dental Group5.0 (163 review)
Orchard Dental Group5.0 (163 review) The Importance of Oral Health Education During Pregnancy for a Healthy Pregnancy
The Importance of Oral Health Education During Pregnancy for a Healthy Pregnancy Best Tips for Brushing Your Teeth Properly for Healthy Gums: Essential Techniques for Oral Health
Best Tips for Brushing Your Teeth Properly for Healthy Gums: Essential Techniques for Oral Health Why Skipping Dental Checkups Can Lead to Bigger Oral Health Problems
Why Skipping Dental Checkups Can Lead to Bigger Oral Health Problems Advantages of Porcelain Dental Restorations
Advantages of Porcelain Dental Restorations How Can Diabetes Cause Tooth and Gum Problems? Preventing and Managing Oral Health Issues
How Can Diabetes Cause Tooth and Gum Problems? Preventing and Managing Oral Health Issues Healthy Habits for Promoting Good Oral Health and Hygiene: Tips for a Healthy Smile
Healthy Habits for Promoting Good Oral Health and Hygiene: Tips for a Healthy Smile