Understanding Gingivitis: Why It Can Occur Even with Great Oral Hygiene
Gingivitis, the early stage of gum disease, often puzzles people who maintain excellent oral hygiene. You might brush twice daily, floss regularly, and visit the dentist, yet still find yourself facing symptoms like red, swollen, or bleeding gums. This situation raises the question: how did I get gingivitis with great oral hygiene? The answer is more complex than simply brushing and flossing. Gingivitis results from a combination of factors, some beyond basic oral care routines.
1. What Exactly Is Gingivitis?
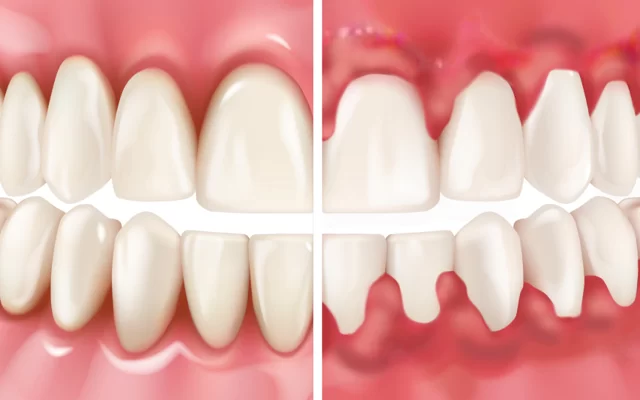
Gingivitis is inflammation of the gums caused primarily by plaque buildup on the teeth. Plaque is a sticky film of bacteria that accumulates daily. If not removed effectively, it irritates the gum tissue, causing redness, swelling, and bleeding. While good oral hygiene dramatically reduces plaque, it doesn’t guarantee complete protection against gingivitis because other factors can contribute.
2. Factors Beyond Brushing: Why Gingivitis Happens Despite Good Oral Care
Even if you are diligent with brushing and flossing, several underlying issues can cause gingivitis:
2.1. Ineffective Brushing and Flossing Techniques
Sometimes, the problem isn’t how often you brush, but how well. Missing spots, especially along the gumline and between teeth, allows plaque to build up. Using a hard-bristled toothbrush or brushing too aggressively can also cause gum irritation, mimicking gingivitis symptoms.
2.2. Hard-to-Reach Areas and Dental Appliances
Areas around wisdom teeth, braces, or dental bridges are prone to plaque accumulation even with good hygiene. These spots require extra attention and sometimes specialized cleaning tools.
2.3. Medical Conditions and Medications
Certain health issues, such as diabetes or immune system disorders, affect gum health. Medications that reduce saliva flow, like antihistamines or antidepressants, can lead to dry mouth, increasing plaque buildup and risk for gingivitis.
2.4. Hormonal Changes
Hormonal fluctuations during pregnancy, puberty, or menopause can make gums more sensitive and prone to inflammation even when oral hygiene is consistent.
2.5. Smoking and Tobacco Use
Smoking weakens your immune system and affects blood flow to the gums, making it harder for your body to fight off infection. This can lead to gingivitis despite your oral care efforts.
2.6. Genetics
Some individuals are genetically predisposed to gum disease. Even with perfect hygiene, their gums might react more severely to plaque.
3. Recognizing the Symptoms Early
Understanding the signs of gingivitis helps in early intervention. Common symptoms include:
- Red, swollen, or tender gums
- Bleeding during brushing or flossing
- Persistent bad breath
- Gum recession or sensitivity
If you notice these signs, even with good oral hygiene, it’s crucial to consult a dental professional promptly.
4. Real-Life Stories: When Good Habits Aren't Enough
Consider Emily, a 32-year-old who brushed twice daily and flossed religiously. Despite this, she experienced bleeding gums. After a dental check-up, she learned she had mild gingivitis caused by her newly placed braces, which made cleaning difficult. Her dentist provided tailored advice and a special interdental brush, which helped her overcome the issue.
Similarly, John, a 45-year-old with well-maintained oral habits, developed gingivitis linked to his uncontrolled diabetes. This highlights how systemic health plays a vital role in gum disease development.
5. Strategies to Prevent and Manage Gingivitis with Great Oral Hygiene
To protect your gums, even with great oral hygiene, consider these advanced strategies:
5.1. Optimize Your Oral Care Routine
Use a soft-bristled toothbrush and fluoride toothpaste. Brush for two minutes, twice daily, ensuring you clean along the gumline gently but thoroughly. Incorporate floss or interdental brushes daily to remove plaque from between teeth.
5.2. Professional Dental Cleanings
Regular dental visits for professional cleanings help remove tartar, hardened plaque that brushing can’t eliminate. Your dentist can detect early signs of gum disease and recommend personalized care.
5.3. Address Medical Conditions
Manage systemic health conditions like diabetes with your healthcare provider, as they directly impact oral health. Discuss medications with your doctor if you experience dry mouth or other side effects that affect gums.
5.4. Lifestyle Adjustments
Quit smoking and reduce alcohol consumption. Eat a balanced diet rich in vitamins C and D, which support gum health. Stay hydrated to promote saliva production, a natural defense against bacteria.
6. When to Seek Immediate Professional Help
If you experience persistent gum bleeding, swelling, or pain despite good oral hygiene, schedule a dental exam. Untreated gingivitis can progress to periodontitis, a severe gum disease leading to tooth loss and other health complications. Early professional intervention can prevent irreversible damage.
Conclusion: Why Gingivitis Can Affect Anyone, Even with Great Oral Hygiene
Gingivitis is multifactorial and can develop despite diligent brushing and flossing. Factors like technique, anatomy, medical conditions, lifestyle, and genetics influence gum health. By understanding these aspects and working closely with dental professionals, you can effectively prevent and manage gingivitis.
For personalized advice and expert care to keep your gums healthy, visit Dentistry Toothtruth, where you can find the best dental services tailored to your needs.







 Westgate Dental Arts3.0 (2 review)
Westgate Dental Arts3.0 (2 review) Coventry Family Dental4.0 (247 review)
Coventry Family Dental4.0 (247 review) Familia Dental3.0 (1028 review)
Familia Dental3.0 (1028 review) Dr. Daniel S. Fife, DDS4.0 (31 review)
Dr. Daniel S. Fife, DDS4.0 (31 review) Dentistry At Suburban Square: Michael I. Wollock, DMD4.0 (1228 review)
Dentistry At Suburban Square: Michael I. Wollock, DMD4.0 (1228 review) Comfort Care Dental4.0 (1156 review)
Comfort Care Dental4.0 (1156 review) The Importance of Oral Health Education During Pregnancy for a Healthy Pregnancy
The Importance of Oral Health Education During Pregnancy for a Healthy Pregnancy Why Skipping Dental Checkups Can Lead to Bigger Oral Health Problems
Why Skipping Dental Checkups Can Lead to Bigger Oral Health Problems Best Tips for Brushing Your Teeth Properly for Healthy Gums: Essential Techniques for Oral Health
Best Tips for Brushing Your Teeth Properly for Healthy Gums: Essential Techniques for Oral Health Advantages of Porcelain Dental Restorations
Advantages of Porcelain Dental Restorations How Can Diabetes Cause Tooth and Gum Problems? Preventing and Managing Oral Health Issues
How Can Diabetes Cause Tooth and Gum Problems? Preventing and Managing Oral Health Issues Healthy Habits for Promoting Good Oral Health and Hygiene: Tips for a Healthy Smile
Healthy Habits for Promoting Good Oral Health and Hygiene: Tips for a Healthy Smile