- 1 - #understanding-infection - Understanding Oral Fungal Infections
- 2 - #early-signs - Early Signs and Common Symptoms
- 3 - #causes-risk - Causes and Risk Factors of Oral Fungal Infections
- 4 - #diagnosis - Diagnosis and Professional Evaluation
- 5 - #treatment-options - Treatment Options for Oral Fungal Infections
- 6 - #real-case - Real Case: Overcoming Chronic Oral Thrush
- 7 - #prevention-tips - Prevention Tips for Stronger Oral Health
- 8 - #when-to-visit - When to Visit Family Dentistry Online for Professional Care
Understanding Oral Fungal Infections
What happens when fungus affects the mouth
Oral fungal infections, commonly known as oral thrush or oral candidiasis, occur when a naturally occurring yeast called Candida albicans grows excessively inside the mouth. This overgrowth leads to visible white patches, discomfort, and sometimes difficulty eating or swallowing. Recognizing the signs of oral fungal infection early can prevent it from spreading or worsening.
Who is most at risk
These infections can affect anyone, but are particularly common in individuals with weakened immune systems, those using inhaled corticosteroids, or patients with diabetes. Smokers and denture wearers also have a higher likelihood of developing fungal growth due to changes in the mouth’s natural environment.
Early Signs and Common Symptoms
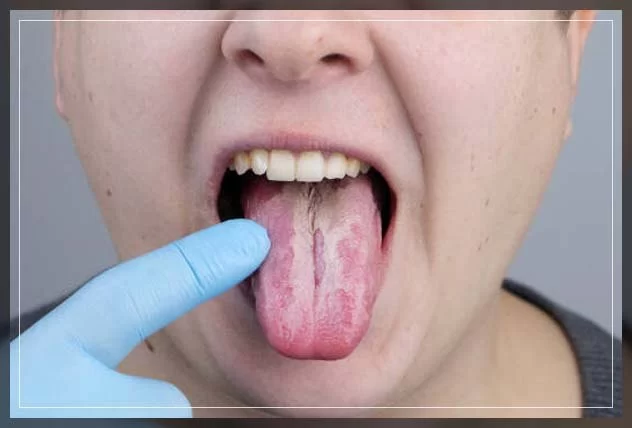
Recognizing the early warning signs
The first noticeable symptom of an oral fungal infection is often white, creamy patches on the tongue, gums, or inner cheeks. These patches can sometimes be wiped away, leaving a red, sore surface underneath. Patients may also experience a cotton-like feeling in the mouth or loss of taste.
Progressive symptoms that require care
As the infection worsens, swallowing may become painful, and the corners of the mouth might crack or become inflamed (a condition called angular cheilitis). Chronic cases can lead to a burning sensation on the tongue and persistent bad breath. Identifying these oral fungal infection symptoms early helps ensure faster recovery.
Causes and Risk Factors of Oral Fungal Infections
Disruption of the mouth’s natural balance
Our mouths naturally maintain a delicate balance of bacteria and yeast. When antibiotics, illness, or poor oral hygiene disrupt this balance, Candida can multiply uncontrollably. The result is inflammation, irritation, and the characteristic white patches of oral thrush.
Underlying medical or lifestyle triggers
Several conditions increase susceptibility, including diabetes, HIV, pregnancy, or use of dentures that aren’t cleaned properly. Even stress and lack of sleep can compromise the immune system, creating an environment where fungus thrives. According to Family Dentistry Online, simple lifestyle adjustments can significantly reduce recurrence risk.
Diagnosis and Professional Evaluation
How dentists confirm the condition
Diagnosing oral fungal infections usually begins with a visual examination. A dentist or healthcare provider will inspect the mouth for characteristic white lesions and may gently scrape them to test for fungal cells under a microscope. In chronic or severe cases, additional lab tests might be needed to rule out systemic conditions.
Why professional care matters
Because oral fungal symptoms often mimic other mouth conditions, self-diagnosis can lead to delays or improper treatment. Consulting professionals at Family Dentistry Online ensures that you receive accurate diagnosis and tailored care for long-term relief.
Treatment Options for Oral Fungal Infections
Medical treatments that work
Treatment depends on the severity of the infection. For mild cases, antifungal mouth rinses or lozenges containing nystatin or clotrimazole are often prescribed. More persistent infections may require oral antifungal medications like fluconazole. Consistency in using these medications is key to full recovery.
At-home care to support healing
Good oral hygiene plays a vital role in recovery. Brushing at least twice a day, replacing toothbrushes regularly, and disinfecting dentures help control fungal regrowth. Avoid sugary foods and alcohol-based mouthwashes, which can feed yeast growth. Family Dentistry Online recommends regular dental cleanings to maintain a healthy oral microbiome.
Real Case: Overcoming Chronic Oral Thrush
Meet Karen’s story
Karen, a 52-year-old patient, struggled with recurring oral thrush for nearly a year. Despite trying over-the-counter remedies, her symptoms kept returning—white patches, sore gums, and constant dryness. Finally, she visited Family Dentistry Online, where a full evaluation revealed underlying diabetes that had gone undiagnosed. Once treated with both antifungal therapy and diabetes management, her symptoms disappeared within weeks.
The lesson from her experience
Karen’s story highlights why addressing both oral and systemic health is essential. Treating symptoms without identifying the root cause often leads to recurrence. A comprehensive dental and medical approach ensures lasting relief.
Prevention Tips for Stronger Oral Health
Simple habits that make a difference
Preventing oral fungal infections starts with maintaining a clean, balanced mouth environment. Brush after meals, rinse with non-alcohol mouthwash, and keep dentures sanitized daily. For inhaler users, rinse the mouth with water after each use to remove medication residue that encourages fungal growth.
Boosting natural defenses
A diet rich in probiotics (like yogurt or kefir), reduced sugar intake, and regular hydration help keep oral yeast in check. Regular dental visits with Family Dentistry Online ensure early detection and professional cleaning that minimizes fungal buildup.
When to Visit Family Dentistry Online for Professional Care
Knowing when to seek help
If you notice persistent white patches, oral soreness, or difficulty swallowing, don’t ignore them. Fungal infections can escalate quickly without treatment. Early evaluation prevents complications and reduces discomfort.
Your trusted partner in oral health
Family Dentistry Online offers expert diagnostic tools, personalized treatment plans, and preventive care programs to manage oral fungal infections effectively. Whether you’re experiencing mild symptoms or chronic recurrence, their team ensures your mouth stays healthy and pain-free.







 Promenade Dental Group and Orthodontics4.0 (347 review)
Promenade Dental Group and Orthodontics4.0 (347 review) Distinctive Smiles of Dublin4.0 (399 review)
Distinctive Smiles of Dublin4.0 (399 review) Sean S Jung DDS5.0 (8 review)
Sean S Jung DDS5.0 (8 review) Faber Orthodontics5.0 (145 review)
Faber Orthodontics5.0 (145 review) Hawthorn Woods Family Dental Care5.0 (535 review)
Hawthorn Woods Family Dental Care5.0 (535 review) Children's Dentistry of Trappe4.0 (491 review)
Children's Dentistry of Trappe4.0 (491 review) The Importance of Oral Health Education During Pregnancy for a Healthy Pregnancy
The Importance of Oral Health Education During Pregnancy for a Healthy Pregnancy Best Tips for Brushing Your Teeth Properly for Healthy Gums: Essential Techniques for Oral Health
Best Tips for Brushing Your Teeth Properly for Healthy Gums: Essential Techniques for Oral Health Why Skipping Dental Checkups Can Lead to Bigger Oral Health Problems
Why Skipping Dental Checkups Can Lead to Bigger Oral Health Problems Advantages of Porcelain Dental Restorations
Advantages of Porcelain Dental Restorations How Can Diabetes Cause Tooth and Gum Problems? Preventing and Managing Oral Health Issues
How Can Diabetes Cause Tooth and Gum Problems? Preventing and Managing Oral Health Issues Healthy Habits for Promoting Good Oral Health and Hygiene: Tips for a Healthy Smile
Healthy Habits for Promoting Good Oral Health and Hygiene: Tips for a Healthy Smile